Oct15

From Factory to Front Door: Why Big Pharma Is Going Direct-to-Patient — and What It Means for Clinicians, Payers and Patients
What if your prescription skipped the pharmacy line and arrived at your doorstep for a flat cash price? That future is here. In 2024–2025, leading manufacturers launched direct-to-patient (DTP) programs that combine transparent cash-pay pricing with telehealth and home delivery. Examples include LillyDirect (Eli Lilly), PfizerForAll, NovoCare Pharmacy (Novo Nordisk), AstraZeneca Direct, AmgenNow, Bristol Myers Squibb’s Eliquis 360 Support, and Novartis’s Cosentyx pilot. This isn’t just a logistics tweak; it’s a shift in who owns the relationship with the patient.
Why now? Three structural forces
GLP-1s changed behavior. Weight-management and diabetes therapies normalized a digital journey—triage → e-prescription → doorstep fulfillment—at a national scale.
Regulatory heat on PBMs. Heightened scrutiny boosted the appeal of disintermediation and simple, cash-pay transparency.
Mature rails. Drugmakers can now plug into telehealth networks, digital pharmacies, and last-mile delivery without rebuilding the stack.
How these programs work
Most offerings are cash-pay with flat monthly pricing, integrated telehealth, and home delivery. For uninsured or high-deductible patients, it can beat today’s copay. The trade-off: purchases outside insurance typically don’t count toward deductibles or annual out-of-pocket limits. Patients should compare direct prices with plan benefits and consider the total annual cost.
Real-world models (non-exhaustive, U.S.)
LillyDirect widened access to Zepbound with single-dose vials and home delivery options.
NovoCare Pharmacy enables cash-pay access to Wegovy and, later, Ozempic via its own online pharmacy and telehealth partners.
PfizerForAll connects consumers to telehealth, prescription fulfillment, and vaccine support for conditions such as migraine, COVID-19, and flu.
AstraZeneca Direct sells Airsupra (asthma) and Farxiga to cash-pay patients and offers FluMist home delivery.
BMS & Pfizer launched Eliquis 360 Support for anticoagulation therapy under a direct-to-patient model.
Novartis is piloting DTP with Cosentyx and exploring direct-to-employer variants.
AmgenNow offers direct access starting with Repatha.
Implications for clinicians
The prescription still originates with a clinician—either a patient’s own doctor or an independent telehealth provider—but continuity can fracture if data stops at the platform’s edge. Practical guardrails help:
Interoperability minimums: a concise start/continue report back to the primary clinician.
Safety protocols: clear inclusion/exclusion criteria, titration, monitoring, and fast escalation to in-person care.
Price transparency: show DTP vs. insured pharmacy costs and deductible implications.
Data governance: explicit, granular consent—no dark patterns.
Implications for patients
Upsides: predictable cash prices, fewer administrative hoops (e.g., prior authorization), and doorstep delivery. Trade-offs: no deductible credit on most cash purchases, risk of fragmented follow-up if clinicians aren’t looped in, and the need to scrutinize privacy practices.
Implications for payers and PBMs
“Cut out the middleman” makes headlines, but the likely outcome is a hybrid approach. Where plan coverage—especially Medicare—beats cash, traditional channels remain superior. DTP thrives where coverage is absent or cumbersome. PBMs that demonstrate transparent clinical and financial value will stay relevant; others will feel pressure from these new rails.
Signals to watch
Platformization: screening → Rx → delivery → engagement in one experience, with add-ons like nutrition and behavioral coaching.
Direct-to-employer pilots layered on top of DTP.
Expansion beyond GLP-1s into cardio-renal, immunology, and respiratory therapies.
Industry aggregation via hubs that list manufacturers’ direct-purchase options.
What leaders should do now
Health systems & payers: Map overlap between DTP cash pricing and your formularies; model leakage and member impact; negotiate data-sharing on adherence and adverse events; educate members on when cash beats coverage—and when it doesn’t.
Clinical leaders: Define minimal datasets for DTP partners (labs, vitals, red flags, dose changes); use DTP to unblock access and schedule prompt follow-ups to maintain cohesive care.
Manufacturers: Treat first-party data as a clinical asset; be honest about the total cost of therapy; co-create real-world evidence with provider networks.
Bottom line
DTP isn’t just a new checkout lane—it’s a redistribution of power along the care journey. Done well—ethically, transparently, and clinically integrated—it can make access simpler and more human. The hard question for every player: what are you willing to give up to earn, and keep, patient trust?
Editor’s note on sourcing: This analysis synthesizes reporting from reputable outlets (e.g., CNBC, Fierce Pharma/Fierce Healthcare), manufacturer press rooms, regulatory materials (e.g., U.S. FTC PBM work and GoodRx enforcement), and clinician surveys (e.g., Sermo). Full source links appear in the companion article file.
Keywords: Customer Experience, Healthcare, Innovation
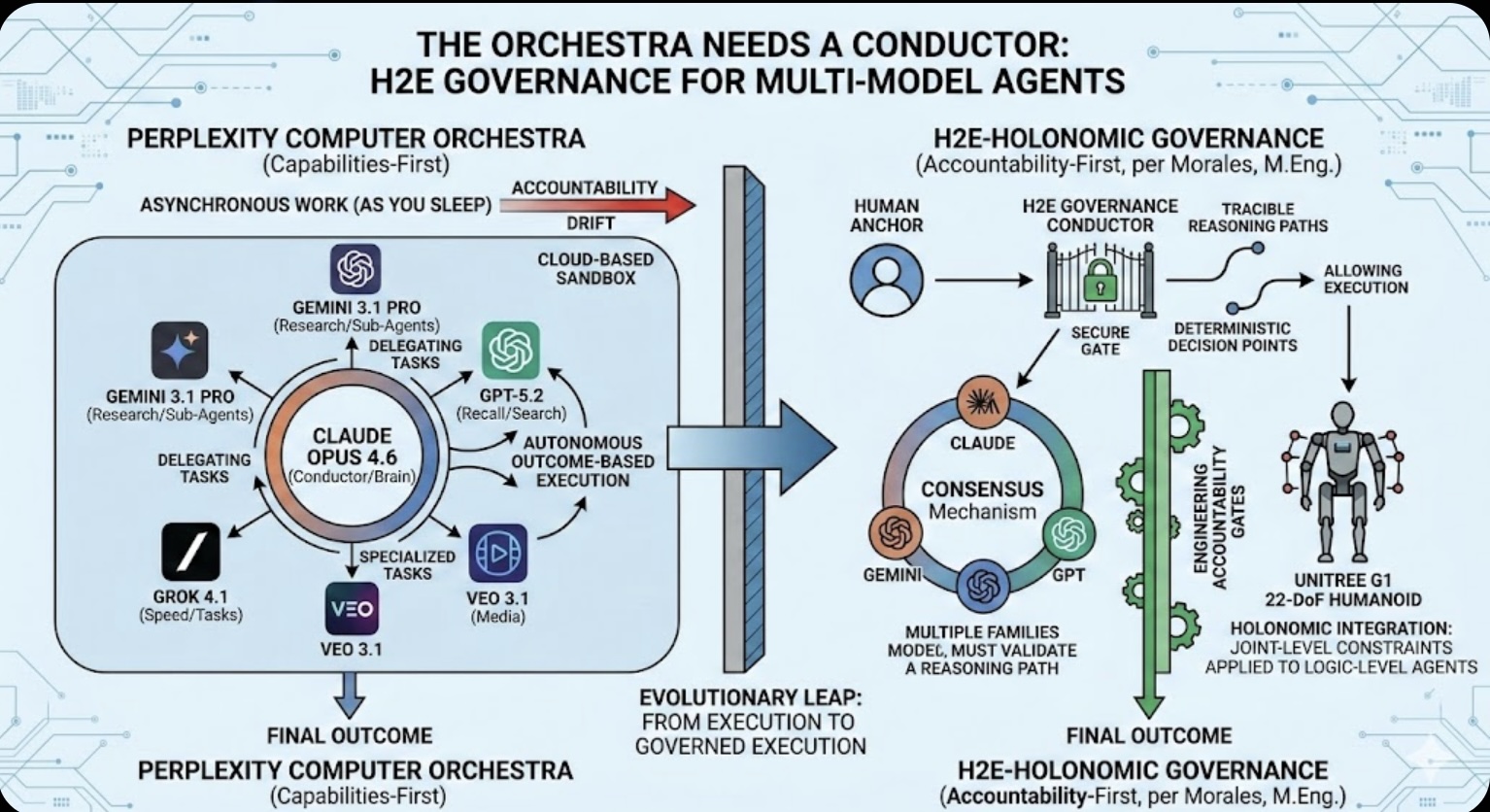 The Orchestra Needs a Conductor: Why Multi-Model Agents Require H2E Governance
The Orchestra Needs a Conductor: Why Multi-Model Agents Require H2E Governance The Role of Memory in Modern-day Business
The Role of Memory in Modern-day Business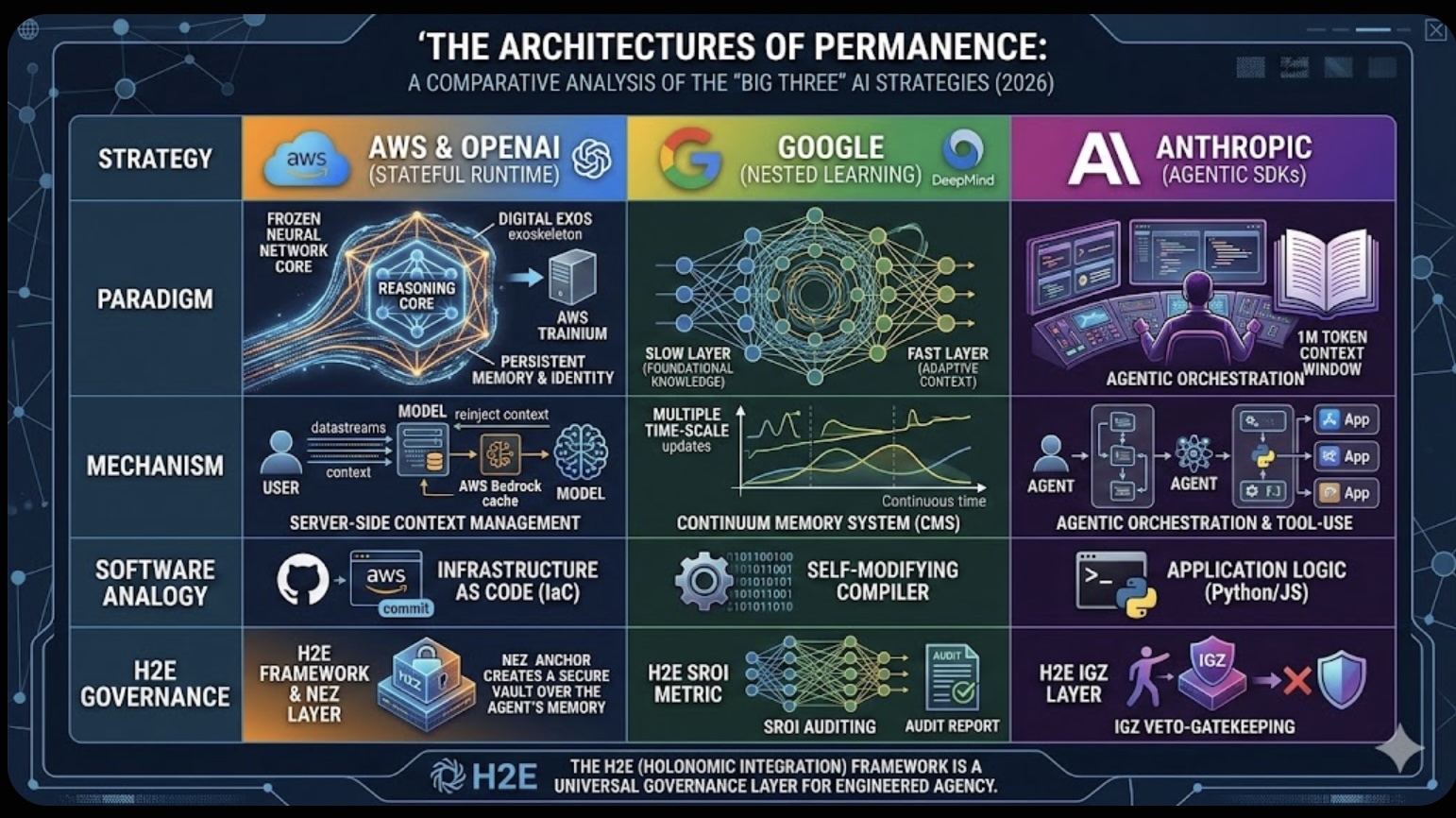 The Architectures of Permanence: A Comparative Analysis of the "Big Three" AI Strategies (2026)
The Architectures of Permanence: A Comparative Analysis of the "Big Three" AI Strategies (2026)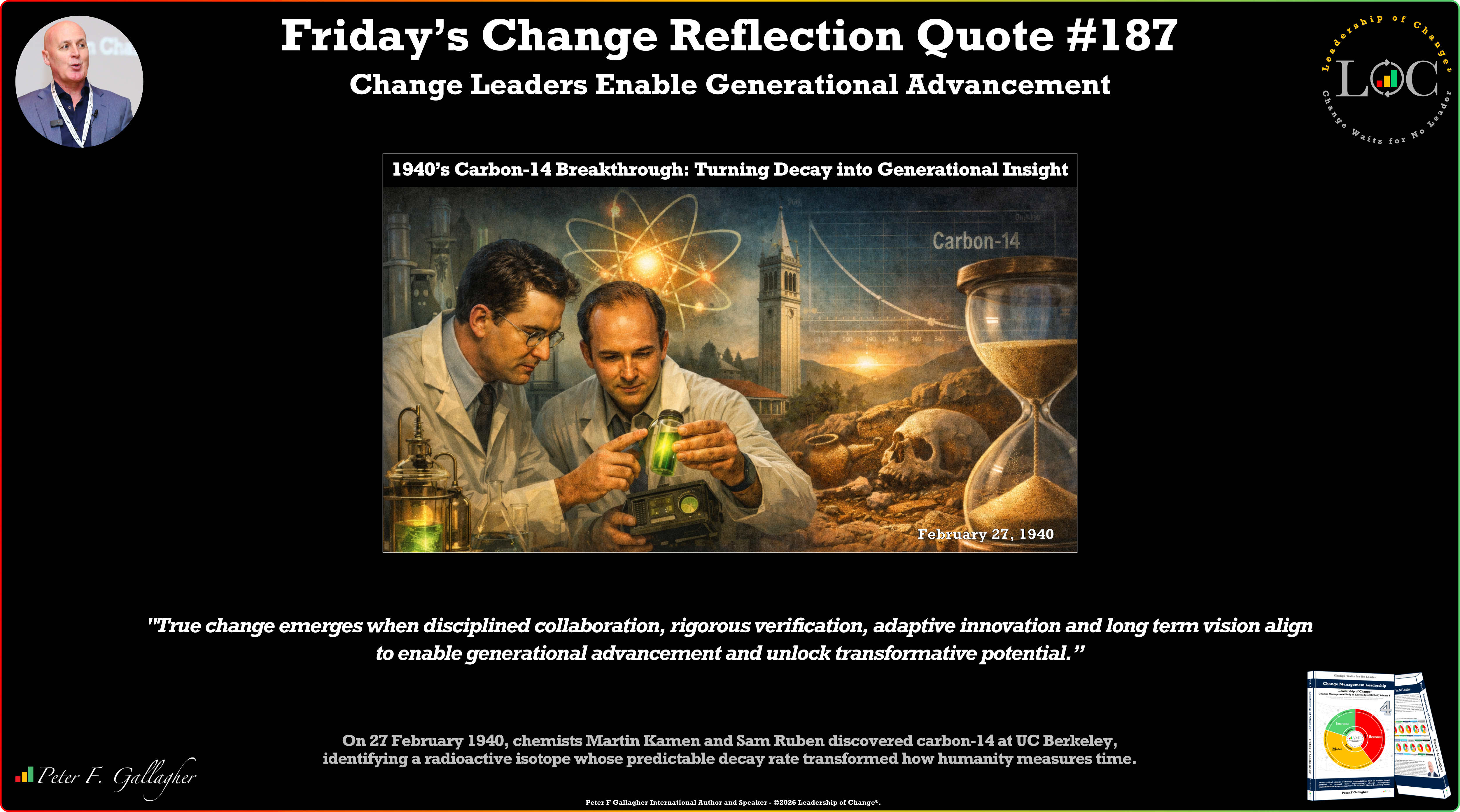 Friday’s Change Reflection Quote - Leadership of Change - Change Leaders Enable Generational Advancement
Friday’s Change Reflection Quote - Leadership of Change - Change Leaders Enable Generational Advancement The Corix Partners Friday Reading List - February 27, 2026
The Corix Partners Friday Reading List - February 27, 2026